Pathogen inactivation (PI) technology inhibits pathogen proliferation by targeting pathogen DNA or RNA with ultraviolet (UV) light illumination, with or without a photosensitizer. While its application in platelet concentrates may provide an effective and reliable method to minimize transfusion-associated infection risk, PI treatment appears to negatively impact platelet quality. There are currently three commercially available systems on the market. Canadian Blood Services is currently involved in The PREPAReS clinical trial (Pathogen Reduction Evaluation & Predictive Analytical Rating Score) to evaluate the clinical effectiveness of the riboflavin /UV light technology (Mirasol, TerumoBCT).
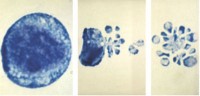
Compared to platelets stored under normal blood banking conditions, PI-treated platelets undergo accelerated apoptosis-like changes, which can be detected as a marked increase in platelet activation, phosphotidylserine (PS) exposure, caspase-3 activation, and phosphorylation of other stress-activated kinases. The expression levels of anti-apoptotic proteins (e.g. Bcl-2 family) and pro-apoptotic proteins (e.g. Bax and Bak) are carefully regulated in order to maintain the apoptosis titter-totter in check. Under normal conditions, anti-apoptotic proteins are expressed/activated to prevent progression to programmed cell death. However, an up-regulated expression level of pro-apoptotic proteins could tilt the titter-totter to mediate apoptosis, triggering activation of downstream caspases for subsequent cell clearance and removal.
Previous study showed that PI treatment appears to increase protein kinase activation in platelets; of note, p38MAPK (p38 mitogen-activated protein kinase) activation showed a greater than two fold increase. This kinase is strongly activated by stress and is known to play important roles in immune response and regulation of cell survival.
Dr. Zhongming Chen, a post-doctoral fellow at Dr. Dana Devine’s laboratory, discovered a novel role of p38MAPK in apoptosis in platelets treated with PI, published in Transfusion. He observed significantly elevated expression of pro-apoptotic proteins, Bax and Bak, in PI-treated platelets compared to those of untreated control. Similarly, downstream caspase-3 and -9 activities also increased markedly in PI-treated platelets, as detected by western blot monitoring caspase cleavage and confirmed with flow cytometry. However, these effects were significantly reduced when an inhibitor of p38MAPK, SB203580 (SB), was added before PI treatment. Other in vitro parameters also suggests that the addition of SB inhibitor prior to PI treatment resulted in a reduction of glucose metabolism , alpha granule release, and PS externalization, indicating that p38MAPK is a major contributor to the progression of apoptosis and is activated in PI-treated platelets. This finding may help to inform future designs for improved PI technology and potentially maximize both platelet safety and quality.
Dr. Zhongming Chen is supported by Canadian Blood Services Postdoctoral Fellowship Program. Reagents, disposables, and the Mirasol instrumentation were provided by TerumoBCT. However, TerumoBCT was not involved in the study design and provided no editorial control over the research or manuscript.
Contribute by Deb Chen, PhD Student in Devine lab, CBR
Front page image from www.flickr.com Zeiss Microscopy