It is not difficult to imagine how blood transfusion saves lives and improves health. But why substitute blood, and more curiously what is it? To answer these questions, let us narrow the term “blood” to red blood cells (RBCs), the oxygen-carrying components of whole blood. With this distinction in mind, to be effective, substitute (or artificial) blood must in the first place be able to carry oxygen, and ideally, it should also be biocompatible with any host regardless of blood type. It should be free of disease causing agents, cost-effectively produced, readily available, and have a long shelf-life. These properties would allow universal access to a safe blood source, which would be especially beneficial in regions where blood reserves suffer from frequent contamination or are in short supply. Although currently there are no FDA approved blood substitutes on the market, progress continues on two major categories of oxygen carriers: perfluorocarbons and hemoglobin-based products.
Perfluorocarbons
In the 1960s, scientists working with lung injuries discovered “liquid ventilation”, where mice were able to survive by spontaneous breathing when their lungs were immersed in liquid perfluorocarbons (PFC). These synthetic PFC liquids are capable of dissolving large amounts of physiologically important gases such as oxygen and carbon dioxide. PFCs were later adapted in emulsion form to serve as artificial blood. Finally in 1989, Fluosol-DA (Green Cross) emerged as the first FDA approved oxygen-carrying blood substitute. Unfortunately, the drug was withdrawn shortly after due to the lack of a clear clinical benefit over the complexities in production and usage. Improved PFC emulsions are currently in development with some having completed phase II clinical trials. PFCs may also have potential non-blood substitute applications. For example, due to their small size (~1/40th of a RBC), they are able to flow through the poor vasculature often found in solid tumors and oxygenate hypoxic cancer cells that are otherwise highly resistant to radiotherapy.
Hemoglobin-based products
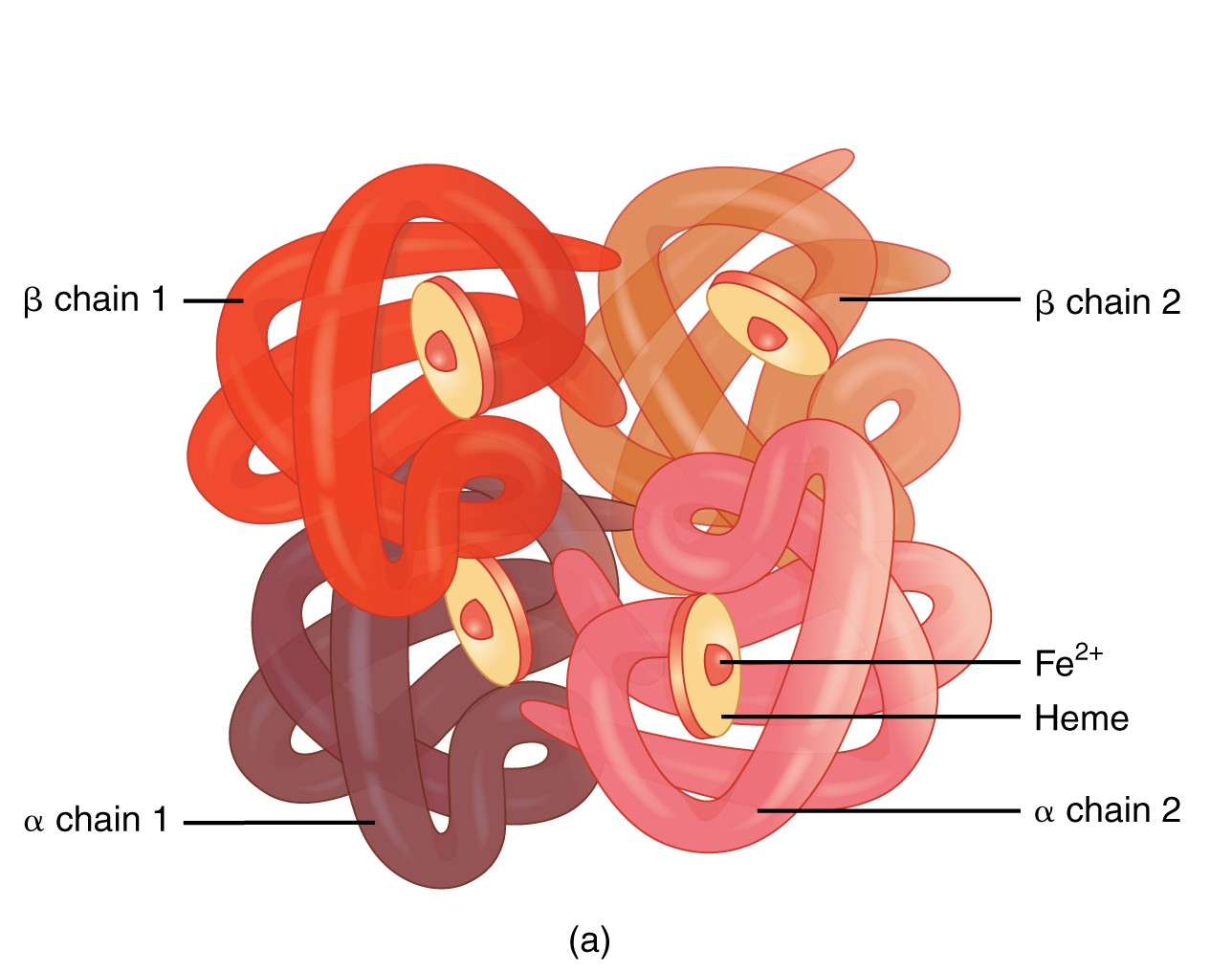
As hemoglobin is the oxygen carrier in RBCs and comprises 33% of the cell mass, its suitability as a blood substitute seems obvious. However, the transfusion of purified hemoglobin poses great challenges. Firstly, native hemoglobin is a tetramer and when introduced naked into the blood stream, it dissociates into a secreted dimeric form that can cause renal toxicity.
Furthermore, free tetrameric hemoglobin is itself toxic because it can enter blood vessel walls and scavenge nitric oxide. As nitric oxide is necessary for the relaxation of blood vessels, its depletion would result in increased blood pressure, which is a side-effect associated with hemoglobin-based oxygen carriers (HBOCs). Common solutions to this problem consist of crosslinking hemoglobin to produce larger polymers (eg. Hemopure; OPK biotech) and polymer coating via site specific PEGylation (eg. Hemospan; Sangart). These increase the stability of free hemoglobin (~20 hrs vs. 30 min) and offset the blood pressure side effects and toxicity. Despite considerable progress in HBOC formulation, these products have yet to successfully complete phase III clinical trials, and in addition face problems related to cost and scalability. Nevertheless, new recombinant technologies could in the future alleviate these concerns.
One should keep in mind that no matter how well made, substitute blood still lacks the other necessary components of whole blood that are vital to its function in the organism. However, despite drawbacks, blood substitutes carry significant advantages that argue for continued research. For example, in contrast to blood that can only be stored up to 42 days, blood substitutes can be stored at ambient temperatures for up to 2 years. Absence of a cellular membrane furthermore means that blood typing is not an issue. As a result, these substitutes are especially useful in trauma settings where blood may not be readily available. With this in mind, the value of artificial blood as a transient solution in trauma and surgery cannot be underestimated, and although a lofty goal, the realization of safe and stable blood substitutes would be of enormous benefit.
Contributed by Solmaz Sobhanifar, PDF in Strynadka Lab at CBR
Front page image from www.wikipedia.org