 By Ido Refaeli, PhD Candidate, McNagny Lab
By Ido Refaeli, PhD Candidate, McNagny Lab
There is an urgent need for curative therapies to treat kidney failure. In 2015, over 21,000 patients in Canada received dialysis to treat kidney failure. Another 2,500 patients received a kidney transplant and 215 died on the waiting list[i].
As part of an ongoing collaboration, the laboratories of Dr. Kelly M. McNagny (UBC, CBR PI) and Dr. Benjamin S. Freedman (University of Washington) have demonstrated that human kidney organoids grown in a culture dish can accurately model kidney development and disease. This work, recently published in Stem Cells[ii], is a culmination of decades of fundamental research into mammalian kidney and stem cell biology. Kidney organoids are multi-cellular aggregates that form structures nearly identical to human kidney nephrons with respect to size, architectural complexity, and cellular makeup. Importantly, these organoids can be generated from patient-derived cells. While there is still a lot of work to be done to optimize this system, human kidney organoid technology promises to expedite kidney research. In the short term, these methods will allow for more rapid screening of drugs. In the future, this technology may provide custom “replacement parts” for patients with failing kidneys.
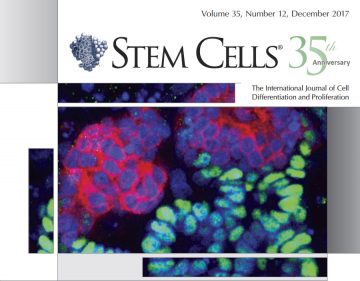
Section of a human kidney organoid
Human kidney organoids are derived from induced pluripotent stem cells (iPSCs). iPSCs are cells which have been genetically reprogrammed to express four key transcription factors that cause them to revert back to a pluripotent state. Once generated in the dish, iPSCs can, in theory, be directed to differentiate into all of the cellular lineages and tissues of the body.
A single human kidney is composed of millions of basic functional units, called nephrons, whose predominant function is to filter blood plasma to form concentrated urine. Because of the kidney’s cellular and architectural complexity, it has long been a challenging endeavour for scientists to study its cells in isolation; the biological function of kidney cells depends on continuous reciprocal interactions with other cells and the interstitial fluids of the kidney.
An especially difficult-to-study kidney cell type is the podocyte. Podocytes are analogous in structure to octopuses: they have a large cell body, which branches out into many little ‘tentacles’ called foot processes that interdigitate with those of neighboring podocytes to form a sieve-like structure through which plasma fluid passes to form urine. The reason for their notoriety is that podocytes can only be found in their native structure in vivo. When they are explanted from the kidney into culture conditions, they dedifferentiate, thereby losing their characteristic cytostructure. And so, experimenting on podocytes in culture is useful to an extent, but ultimately, critical findings have to be validated in animal models.
Podocytopathies are a group of kidney diseases that primarily affect podocytes. For many individuals diagnosed with a podocytopathy, this very likely means a one-way-ticket to end-stage kidney disease. Part of the reason why there aren’t many treatments for podocytopathies today is because of our inability to study these cells in isolation.
In fact, kidney research has largely been conducted using human subjects, rodents or other animal models. Unfortunately, it is logistically difficult to scale the number of human subjects needed to achieve population-level statistical significance in a study. Moreover, there are unavoidable species-specific differences between rodents and humans that can sometimes hinder the translation of insights from animal models to the clinic. Missing for a long time in the field was a technology that would catalyze nephrology research by being both higher throughput and species-specific.
In this recent work, the multi-disciplinary research team showed that podocytes from kidney organoids can recapitulate most of the developmental progression and structural characteristics of podocytes found in both mouse and human kidneys. Next, they generated mutant organoids using the CRISPR/Cas9 gene-editing system and compared them to mice bearing the same mutation. What they found opens up many new opportunities for the use of kidney organoids as a model system; they showed that mutant podocytes from human kidney organoids exhibit near-identical phenotypes to mutated podocytes in the mouse. This finding demonstrates that human kidney organoids are a relevant system in which to model podocyte biology and disease. That they are derived from human cells circumvents the issue of species-specificity, and since they are relatively cheap and readily accessible to experimental manipulation, human kidney organoids offer a high throughput model system.
[i] Canadian Institute for Health Information https://secure.cihi.ca/estore/productFamily.htm?locale=en&pf=PFC3380
[ii] Kim YK, Refaeli I, and Brooks CR et al. Stem Cells 2017;35:2366–2378. http://rdcu.be/FQlQ/


