 By Deb Chen, PhD Candidate in Devine Lab, CBR
By Deb Chen, PhD Candidate in Devine Lab, CBR
Bacterial contamination and emerging pathogens pose a great risk to the safety of the blood supply. In order to minimize potential risk of transfusion-transmitted diseases, routine screening and rigorous testing are performed. However, blood banks can only screen and test for known infectious risks and agents, respectively. Moreover, these tests may not be able to reliably detect the presence of infection in a donor during the “window” of incubation period, which consequently compromise transfusion safety.
Pathogen inactivation (PI) technologies are used to inhibit pathogen proliferation and to prevent the likelihood of disease transmission. This has to be balanced with preserving the adequate quality of cells and proteins in the blood product to improve transfusion recipient outcome. PI technologies are currently used withplatelet and plasma components to increase overall product safety. Gamma-irradiation is routinely used in red blood cell (RBC) to increase product safety for vulnerable recipient populations. Applications to RBC concentrates have been shown to be an alternative to gamma-irradiation to prevent transfusion-associated graft-versus-host disease. Compared to individual component treatment, application of PI technologies to whole blood (prior to component separation and production) promises significant time and cost savings to the blood banking community.
Dr. Peter Schubert, a Research Associate and Manager of Dr. Dana Devine’s Laboratory at Centre for Blood Research (CBR), collaborated with an industry partner, TerumoBCT, to investigate the impact of PI by riboflavin and UV light in whole blood on the quality of all blood components, throughout storage under normal blood bank conditions. Their study, published in Transfusion, showed that, in general, PI treatment compromised in vitro quality parameters in all blood components compared to those left untreated.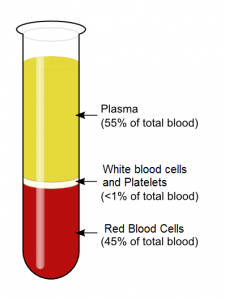
Red blood cells showed accelerated storage-related deterioration. Notably, at the end of a 42-day storage period, RBC rupture levels exceeded the Canadian standards for RBC quality, suggesting a reduced shelf-life for PI-treated RBCs. Although FXIII and VWF activities remained unaffected, PI treatment resulted in a 10% to 44% reduction in the activity of multiple coagulation proteins. The residual activity level of FVIII coagulation factor in the treated units were at or below the Canadian regulatory standard in 75% of plasma units tested, indicating that manufacturing transfusion plasma products by PI of whole blood may be problematic. Interestingly, platelets derived from whole blood PI treatment were less impacted than platelets treated at the component level.
Undoubtedly, whole blood PI treatment appeals greatly to the blood banking community with its benefits of huge time and cost savings. This study shows that whole blood PI treatment degrades the in vitro quality of individual components compared to those left untreated, as is expected from any method of PI. It also suggests that some in vitro parameters may require changes to the length of shelf-life (e.g., RBC), while others are acceptable or even favorable, as in the case of platelets.
The bigger question is – how do these in vitro changes influence the clinical outcome? Studies have reported comparable inactivation levels of white blood cells, bacteria, parasites, and viruses at the whole blood level and the final component level (e.g., platelets and plasma). Current clinical trials (e.g., IMPROVE II and AIMS Study) are further assessing the impact of changes to RBC quality induced by PI-treatment on clinical efficacy.
Taken together, these findings suggest that whole blood treatment with riboflavin and UV light may be a practical alternative to obtain safe blood components in a one-step procedure. This would contribute to a cost reduction compared to individual component treatment.



