 By Erika Siren, PhD Student in Jay Kizhakkedathu Lab
By Erika Siren, PhD Student in Jay Kizhakkedathu Lab
Beta-thalassemia is a genetic blood condition where affected individuals are unable to produce sufficient levels of normal red blood cells. While advances in gene therapy hold promise for a cure(read more about it here), they remain in early stages of development. Currently, the primary treatment for individuals with Beta-thalassemia major is having regular blood transfusions coupled with Iron Chelation Therapy (ICT). ICT is required, as repeated blood transfusions cause iron overload leading to organ dysfunction. The gold standard of ICT is a small molecule, called desferrioxamine, or DFO (inset). However, the short half-life of the drug (20 minutes in humans) demands 8-12 subcutaneous injections per day.
In order to reduce the burden of rigorous ICT regimens, Jasmine Hamilton, a recent alumnus from the Kizhakkedathu research group at the CBR, developed a high molecular weight scaffold for DFO that increases both loading of the drug per injection, as well as the half-life of the drug. A thousand-fold smaller than a red blood cell, a single scaffold serves as a nanocarrier for hundreds of DFO molecules. Once attached to the structure, the DFO conjugate exhibited significantly reduced plasma clearance times, effectively becoming an ultra-long circulating desferroxamine (ULC-DFO).
In the latest issue of Biomaterials, this nanocarrier was shown to effectively clear iron overload in mouse models using only a single injection per week. Despite circulation times of over 16 hours, no detrimental organ accumulation or toxicity related to the introduction of the nanocarrier were reported.
The significant reduction in dosing frequency with ULC-DFO compared to monomeric DFO illustrates great promise in improving the quality of life for patients with beta-thalassemia major.
When asked, “What’s next for ULC-DFO nanocarriers?”, Dr. Kizhakkedathu stated that they are looking towards making biodegradable scaffolds for DFO. These scaffolds will have the same effect of ULC-DFO without the accumulation of the scaffold material in vivo.
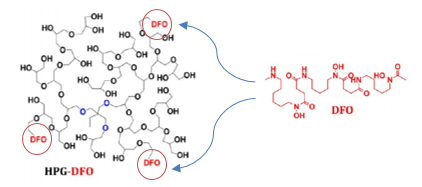
Figure 1. A drug currently used to treat beta-thalessemia, DFO, is attached to the HPG nanocarrier


