Asthma is a common, increasingly frequent, chronic inflammatory disease of the airways that affects over 100 million people worldwide. It is associated with shortness of breath, coughing and wheezing, and necessitates the use of puffers by millions of children. This treatment is required to prevent considerable short- and long-term morbidity and mortality.
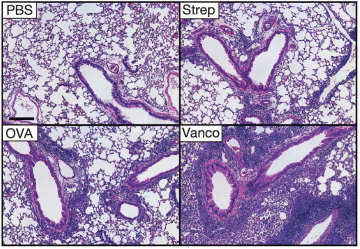
Lung sections from mice reveals worse evidence of asthma after vancomycin treatment
Although the cause of asthma remains a mystery, it has long been believed that improved sanitation methods and the broad use of antibiotics has adversely affected the development of the immune system. This reduced exposure to bacteria, the so-called “hygiene” hypothesis, renders children at increased risk of developing the disorder. This hypothesis has, however, not been tested.
Since the gut is a normal reservoir for bacteria, the research teams of CBR investigator, Dr. Kelly McNagny (Biomedical Research Centre) and Dr. Brett Finlay (Dept of Microbiology and Immunology; Michael Smith Laboratories) collaborated to evaluate the role of antibiotics and gut microbes on the development of asthma.
Using a mouse model of allergic asthma, they found that when the antibiotic vancomycin is used at low dose early in life, it profoundly alters the bacterial community in the gut, and markedly increases the incidence and severity of the asthma. Interestingly, when mice were treated with vancomycin as adults, the asthma rates were not affected. Moreover, not all antibiotics had the same effect, i.e. streptomycin did not alter asthma rates when given at any time, indicating that only specific bacteria influence the development of allergic asthma.
Overall, these intriguing findings, published in the journal EMBO Reports (2012 May 1;13(5):440-7) strongly suggest that certain bacteria are critical during childhood in promoting development of a robust immune system that can protect against allergic asthma. Extension of this work to humans will be fascinating and important. These findings will hopefully lead to novel insights into the interplay between bacteria and the immune system, the development of novel therapies for asthma, and the clinical selection and use of antibiotics that do not ultimately contribute to asthma.
For the whole story, please click here.



Comments are closed, but trackbacks and pingbacks are open.