 By Emel Islamzada, Graduate Student, Ma Lab
By Emel Islamzada, Graduate Student, Ma Lab
Donated red blood cell units are a vital component of patient care, supporting patients with a wide variety of disorders. These include severe kidney disease, hemoglobin and bleeding disorders, bone marrow failure syndromes and recovery from chemotherapy. Some patients, like those with thalassemia and sickle cell anemia, have a lifelong dependency on blood donations. However, not all blood units are the same, and the benefit they can deliver to a patient can vary from unit to unit. Certain donors have red blood cells that will last in cold storage and in the circulation of a recipient for longer. Unfortunately, there is no method to identify these donors or predict which unit will confer maximal benefit to a particular patient after transfusion.
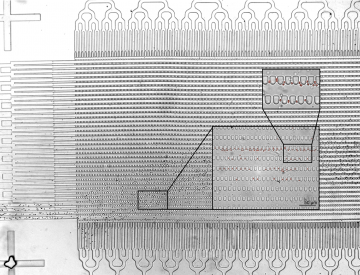
Image of RBCs being sorted through the device based on deformability
One factor that will affect the post-transfusion circulation time is the deformability of a red blood cell. Red blood cells are the ballerinas of the cell world, being able to fold and deform, or squeeze, through openings much smaller than their size as they travel through the vasculature delivering oxygen. The deformability of red blood cells is central to their proper function. During cold storage, the cells gradually lose their ability to deform. The cells that are less deformable won’t be able to transport oxygen efficiently and will be cleared from the recipient’s circulation shortly after transfusion. Being able to accurately measure deformability of red blood cells would allow blood operators to distinguish donors whose red blood cells have a short storage and circulation time, from the “super-storers” or donors whose red blood cells store well in the cold and also will circulate for longer times in the recipient after transfusion.

The Multi Scale Design Lab
In the Multi Scale Design Lab at the Centre for Blood Research, under the supervision of Dr. Hongshen Ma, and in collaboration with Dr. Mark Scott, a Canadian Blood Services senior scientist, we have developed a unique microfluidic ratchet device that sensitively and accurately quantifies the deformability or “squeezability” of red blood cells in donated units. The device sorts red blood cells based on how well they can squeeze through a series of very small constrictions, the latter which mimic the blood vessels and small openings in the circulation. Once the cells are sorted in the device, an individual deformability curve or a “deformability signature” can be generated. This can be compared between units to see which have red blood cells that best retain their ability to deform. We aim to use this device to create an individual deformability profile of red blood cells from donated blood and predict their circulation times in the recipient.
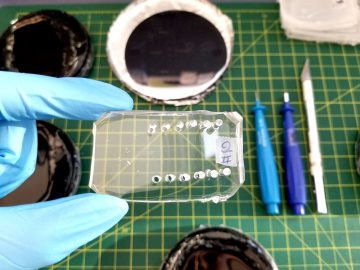
Manufacture of the microfluidic ratchet device
So far, we have tested red blood cells from eight donors, and found two among them whose red blood cells are minimally affected by cold storage. Thus, the device was able to identify potential “super-storers”, i.e. donors with red blood cells that exhibit very little time-dependent changes in their deformability. We also show that the deformability profile of an individual donor stays fairly constant with repeated donations. Another very exciting finding was that all donors’ red blood cells have unique deformability profiles, and very different responses to cold storage.
Our study illustrates the potential of deformability-based sorting to identify those “super-storers” who have extra hardy red blood cells. Although we are excited by these findings, we appreciate that there is still a lot of work ahead to confirm our results with a much larger sample set. This will be enabled by support from the Canadian Blood Services. We are also pursuing studies with animal models to better understand the relationship between red cell deformability and post-transfusion clearance rate.
Emel conducting an experiment with the device at the Centre for Blood Research
This novel method has the potential to enable doctors to, for example, select “super-storer” units for chronic transfusion recipients. All donated blood is valuable, and matching units to the recipients who will benefit most from them could reduce the number of total transfusions needed by these patients and increase the overall blood supply.
I thank Canadian Blood Services for supporting my graduate studies through the Graduate Student Fellowship Award. It is exciting and rewarding to be part of this research stream, and potentially help to improve blood transfusion practices in the future.


