Ulcerative colitis is a chronic inflammatory bowel disease that is increasing in prevalence, and is characterized by weight loss, diarrhea, bleeding and fever. The disorder features invasion of the intestinal wall with the white blood cells, distortion of normal glanduloar structures, and multiple abscesses. Although it is known that altered regulation of the immune response leads to inflammation and tissue damage, the underlying mechanisms have remained a mystery. In studies led by CBR investigator Dr. Kelly McNagny at the Biomedical Research Centre, CBR-funded trainees, Steven Maltby and Michael Hughes have uncovered a novel paradigm to explain disease progression, thereby providing insights into urgently needed new therapeutic strategies
Ulcerative colitis (UC) is an inflammatory bowel disease that is becoming increasingly prevalent in Western society, however, little is known about its etiology. In patients with UC, dysregulation of immune responses in the lining cells of the bowel – the mucosal cells – leads to tissue damage, severe weight loss, diarrhea, bleeding, fever and shortening of the colon. Some insights have been gained into the mechanisms underlying disease progression through studies in mouse models. Intriguingly, a number of recent studies have highlighted an emerging role for eosinophils, a relatively understudied population of blood inflammatory cells, in the development and progression of UC.
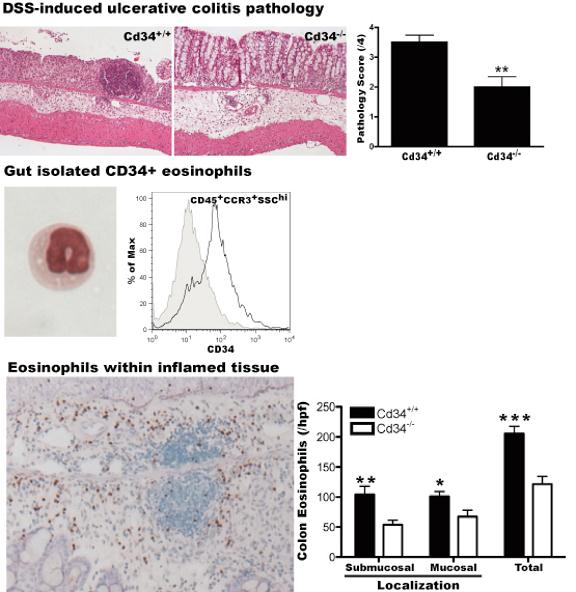
CBR member Dr. Kelly McNagny and his research group at the Biomedical Research Centre have now shown that eosinophil trafficking is a key step in the development of UC in a mouse model of this disease. Previously, Dr. McNagny’s team discovered that the cell surface protein, CD34 plays an important role in facilitating the movement and trafficking of eosinophils, in an allergic asthma model. Based on these findings, CBR-funded trainees, Steven Maltby and Michael Hughes undertook a new study to determine the role of CD34 in a dextran sulfate sodium (DSS)-induced mouse model of ulcerative colitis. Their findings, recently published in The American Journal of Pathology, demonstrated that animals lacking expression of the molecule, CD34, were protected from disease. CD34 expression in inflamed colon tissues was mainly found on infiltrating eosinophils and loss of CD34 resulted in decreased eosinophil infiltration into the colon and ameliorated disease. These studies demonstrate a key role for CD34 in optimal eosinophil migration and suggest that CD34 or eosinophil trafficking might be attractive therapeutic tagets for UC.
This study garnered the attention of inflammatory disease expert, Dr. Rick Stevens (Brigham and Women’s Hospital, Harvard Medical School), who recommended it as a Faculty of 1000 manuscript. In his review, Dr. Stevens states that “The Maltby et al. study reveals an unexpected critical role for CD34 expressing cells in DSS-induced colitis, which changes the paradigm of the disorder and thereby the area of emphasis for future studies.”
This research was supported by national operating grants from the CIHR and the AllerGen Network NCE. Study participants Steven Maltby and Michael R. Hughes each hold CIHR and Heart and Stroke Foundation of Canada Transfusion Science Fellowships from the CBR and Matthew Gold holds funding from the CIHR and Michael Smith Foundation of Health Research Transplantation Training Program. Kelly M. McNagny is a Michael Smith Foundation for Health Research Scholar (Senior) and CBR Member.
Get the whole story in American Journal of Pathology (2010) 177, 1244-1254


